Whenever the UK media discusses the NHS, more often than not it is talking about the NHS in England, rather than all four nations, although it rarely makes that distinction.
As the Welsh Government develops plans to change the way that the NHS is governed, we thought it may be timely to reflect on how different the health system in Wales really is, and what the planned changes might mean.
Who manages NHS services in Wales?
Since 2009, health services in Wales have been managed and delivered by seven local health boards (LHBs). These Boards are both commissioners and providers of services in their areas, with responsibility for the health of their local population.
This means that they deliver or commission the full range of health services, including hospital-based, mental health and community services; and they contract with GPs, pharmacists, opticians and dentists for the provision of local primary care services.
Unlike the other six, the Powys Health Board doesn’t have a large District General Hospital. As a result it commissions many of its hospital services from across the border in England, and is much less involved in directly providing secondary hospital care.
This structure contrasts with elsewhere in the UK; in England the Health and Social Care Act 2012 maintained the split between commissioning (led locally by 191 Clinical Commissioning Groups and nationally by NHS England) and service provision led primarily by over 200 NHS Trusts and NHS Foundation Trusts. Scotland has a system of integrated health boards similar to Wales; in Northern Ireland a single government department oversees health and social care and the Health Services Executive is responsible for a health service that is delivered by a combination of public, private and voluntary providers.
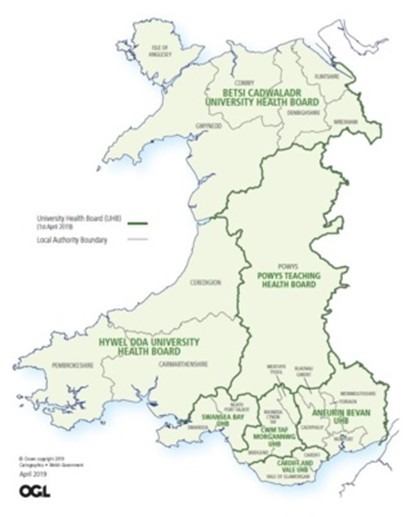 Local Health Boards in NHS Wales from 1 April 2019
Local Health Boards in NHS Wales from 1 April 2019
Alongside the LHBs, there are three NHS Trusts in Wales, each with an all-Wales remit:
There are additionally a range of national bodies with responsibility for aspects of IT and some ‘shared services’ (e.g. payroll, estates, legal and procurement). Health Education and Improvement Wales oversees the planning, education, training and development of the Welsh health workforce. The NHS Wales Delivery Unit provides support to Welsh Government in monitoring and managing performance delivery across NHS Wales and 1000 Lives Improvement supports improvements in health and social care across Wales.
The role of Welsh Government
The Chief Executive of NHS Wales is responsible currently for the strategic leadership and management of all NHS Wales services, but is also the Director General of the Welsh Government Health and Social Services Group. However, this will be changing in the near future as Welsh Government have recently committed to the establishment of a new and distinct NHS Executive for Wales. This is in response to the recommendation from the 2018 Parliamentary Review of Health and Social Care in Wales, which called for ‘a strengthened executive centre’ and ‘a clearer separation between the NHS Wales national executive function, and the national civil service function’. This in turn echoed the findings of the OECD in 2016, which stated that in Welsh healthcare ‘A stronger central guiding hand is now needed to play a more prescriptive role’.
How are services planned and funded?
Wales no longer has a market-based system like England but focuses instead on a more planning-based approach, based around 3-year Integrated Medium Term Plans. There are similarities between commissioning and planning; both are about strategic goals, making choices and shaping current and future services. However, Wales doesn’t use money to drive change in the system in the same way as England: England has a payment by results tariff-based system, with commissioners holding the budget, whereas LHBs and Welsh NHS Trusts receive specific core funding allocations based primarily on the size and make-up of their local population.
How is NHS Wales regulated and monitored?
Regulation and inspection of NHS and independent healthcare services is led by Healthcare Inspectorate Wales (HIW). HIW can identify areas for improvement where providers are failing to meet standards. HIW is also one element – along with the Welsh Government and Wales Audit Office – of the tripartite NHS Wales escalation and intervention arrangements which scrutinise the overall position of each health board and NHS trust in respect of quality, service performance and financial management.
This is different from England, which has arguably a more interventionist regime; the Care Quality Commission (CQC) inspects both health and social care services, and has strong powers of intervention, including the ability to issue warning notices, impose fines or place providers in special measures. Alongside the CQC, NHS Improvement is responsible for overseeing NHS Trusts, foundation trusts and independent providers of NHS-funded care, but is also able to intervene.
At the same time, Wales has until now retained Community Health Councils (CHCs) – the independent statutory bodies representing the interests of patients and the public, and who also inspect local NHS services. There are 7 CHCs, coterminous with the local health boards. However, Welsh Government have recently set out proposals under the Health and Social Care (Quality and Engagement) (Wales) Bill to replace CHCs with a new all-Wales Citizen Voice Body that is intended to represent the interests of people across both health and social care.
In England, patients locally and nationally are represented by Healthwatch, whereas the Scottish Health Council and The Patient and Client Council in Northern Ireland provide independent voices for patients, clients, carers and communities on both health and social care issues. However, none of these bodies have the range of statutory powers available to CHCs.
What are the challenges?
The new NHS Executive will be established at a challenging and interesting time. Wales faces many of the same issues confronting health services across the UK and beyond: workforce and recruitment, financial pressures, long waiting times, increasing demand on services, the growing public health challenges linked to chronic disease and unhealthy lifestyles, and achieving the right mix and shape of services.
There are also distinct governance and quality issues. Betsi Cadwaladr LHB has been in special measures since 2015, with several other LHBs under targeted intervention or enhanced monitoring. The effectiveness of the tripartite and wider quality governance arrangements has been called into question by the serious concerns around maternity services in Cwm Taf LHB.
Similarly, the proposals within the Health and Social Care (Quality and Engagement) (Wales) Bill to replace CHCs have aroused controversy, with concerns about the loss of rights to inspect hospitals and GP surgeries, the absence of clear structures to ensure local representation and the potential loss of a voice on controversial service change proposals. There’s a lot to be tackled.